Abstract
Glomangiomas are rare and benign tumors of glomus bodies, specialized vascular structures found in the skin. Both sporadic and familial types have been reported. The clinical diagnosis of glomangioma can be confusing and easily missed. Hence, a histological diagnosis is necessary. We report the first case of regional glomangioma diagnosed in our clinic, which was successfully managed by surgical excision.
Introduction
Glomangiomas are benign hamartomatous skin tumors characterized by dilated vascular channels surrounded by glomus cells [1]. Pierre Masson, in the early twenties, described the neuromyoarterial glomus, which he subsequently called neurovascular glomus, and associated tumors [2]. In 1935, Bailey coined the term glomangioma, which currently refers to variants of glomus tumors characterized by wide vascular lumina [3]. Glomus tumors consist of cells resembling the smooth muscle cells of the normal glomus body [4]. Glomangiomas are clinically different from glomus tumors as they occur in childhood and adolescence and are usually asymptomatic [5]. Glomangiomas are also often multifocal and do not have a predilection for the subungual region [5]. The lesions are usually nodular, blue or purple in color, and poorly compressible [6]. Multiple glomangiomas comprise 10% of all glomus tumors and are considered to be rare [7]. Our case is that of a young Nigerian woman diagnosed with glomangioma based on clinical and histological findings.
Case Presentation
A 27-year-old female patient presented at the dermatology clinic with a history of multiple skin lesions on the posterior part of the left thigh of 4 years duration. The lesions were compressible and mildly painful. They had gradually increased in size over the years but were restricted to the posterior aspect of the thigh. There were no similar lesions in other regions of the body. She had no significant past medical history. No known history of similar lesions in any of the first-degree relatives. She is not diabetic or hypertensive and had no other symptoms on review of the systems.
Examination of the lesions showed four soft nodules of varying sizes at the posterior part of the left upper thigh with mild tenderness (Figure 1). The nodules were partially compressible (reduced in size with pressure). A solitary hyperpigmented patch (caféau lait spot) at the posterior aspect of the left thigh was also noted (Figure 1). There were no axillary freckles. The mucosal membranes, hair, and nails appeared normal. Other aspects of physical examination revealed no remarkable findings.

An initial clinical diagnosis of Neurofibromatosis (Type 1) was made.
An excisional biopsy was, however, done for two of the nodules on the left thigh.
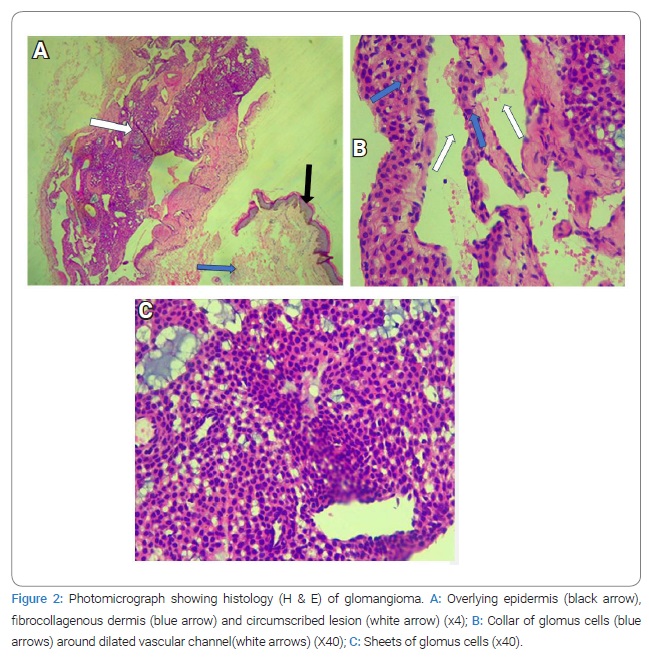
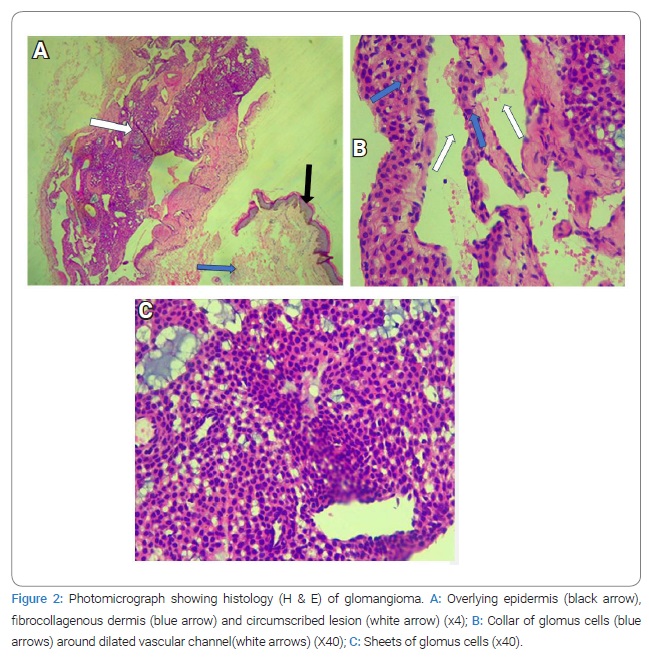
The biopsy specimen consisted of a formalin-fixed single piece of greyish white tissue with overlying negroid skin, soft in consistency, and measured 8 mm x 5 mm x 4 mm. Cut section showed a greyish white surface with a circumscribed brownish area. Histological examination (H & E stain) in (Figure 2) below revealed a keratinizing stratified squamous epithelium overlying a fibro collagenous dermis within which lies a well-circumscribed lesion, composed of sheets and cords of uniform small round to oval shaped cells (glomus) with centrally located bland nuclei and light eosinophilic cytoplasm. These cells are seen to be forming collars around a network of dilated vascular channels, and around the cells are punched out spaces with wispy substance. Also seen are foci of smooth muscles and fibroblasts.
There were no features suggestive of a neurofibroma. A final diagnosis of glomangioma was made. The patient was counseled, and the remaining lesions were subsequently excised. There have been no further concerns or recurrence within four months of excision, and the patient is to be followed up for a minimum of 12 months.
Discussion
Glomangiomas (Glomuvenous malformations) are variants of glomus tumors characterized by hyperplasia of the glomus body, which is a component of the skin and a special arteriovenous anastomosis that contributes to the thermoregulatory function of the skin [8].
Glomangiomas are rare and benign hamartomas. They accounted for 5.1% of the total cohort of patients with venous anomalies [9]. The subungual type, which is rarer, unlike glomus tumors, is most commonly present in female patients [8,10]. Multiple glomangiomas, although rare, comprised about 10% of all glomus tumors [7]. This is the first case of glomangioma diagnosed in our clinic.
Most cases of glomangiomas are sporadic, but familial cases with autosomal dominant inheritance patterns have been reported [5]. These have been mapped to 1p21-22 with loss-of-function mutations in the cytoplasmic protein glomulin as a likely cause [11]. Boon et al. reported familial glomangioma in 63.8% of glomangioma patients [9]. There was no history of similar lesions in first-degree relatives of our patient.
There are three different variants of glomangiomas. The regional type is usually blue-to-purple, partially compressible papules or nodules with a cobblestone-like appearance that are grouped and confined to a specific area, most commonly the extremities. The disseminated variant is made up of multiple lesions that are distributed all over the body. Finally, congenital plaque-like glomus tumors consist of either grouped papules that coalesce to form indurated plaques or clusters of discrete nodules [12,13]. Our patient presented with the regional type of glomangioma that was limited to the left lower limb, even though regional lesions are generally commoner in the upper limbs.
Furthermore, glomangiomas are tender when compressed, and associated pain may be exacerbated by menstruation and pregnancy. In our patient, the lesions were painful when compressed, but the associated pain was not related to menstruation or pregnancy. Extra-cutaneous involvement has been reported in the gastrointestinal tract, liver, pancreas, nerves, trachea, mediastinum, bone, and ovary [14]. These tumors may arise from pluripotent mesenchymal perivascular cells or ordinary smooth muscle cells that can differentiate into glomus cells [9,12,15]. This patient had no clinical features suggestive of extra-cutaneous involvement.
Clinical diagnosis of glomangiomas remains a challenge despite clear pathologic features. They typically present at birth or during childhood as purple skin lesions with a cobblestone pattern that grows over time [16]. Our patient noticed her lesions when she was 23 years of age. It is possible that lesions had been sub-clinical and were only noticed at the time of significant growth. On average, the duration of symptoms to the time of diagnosis is reported to be 7 years–11 years, and the mean amount of physician consultations before a diagnosis is 2.6 [15]. Our patient’s symptoms started four years prior to her review. She had visited different general physicians without a clear diagnosis or treatment plan. Referring physicians are noted to make a correct diagnosis in only 18.2% of cases. Thus, the proposed rarity of the condition may be attributable to either a delay or a dearth in making an accurate diagnosis [15]. According to Boon et al., glomangiomas can be clinically differentiated from venous malformations using these features: cobblestone-like bluish purple or dark blue lesion with minor hyperkeratosis, pain on compression of the lesions, absence of phlebolits, absence of shrinking with external pressure or in dependent position and absence of pain with hormonal modulation (puberty, menstruation, pregnancy or antiovulation drugs) as opposed to venous malformations [9]. Clinical differential diagnosis of glomangioma includes venous malformations, Blue Rubber Bleb Venous Syndrome (BRBNS), hemangiomas, myopericytoma, and Maffucci syndrome [17]. Our patient’s initial provisional diagnosis of type 1 neurofibromatosis was made because of a solitary hyperpigmented patch (café au lait patch) near the glomangiomas. Although the co-existance of glomangioma and type 1 neurofibromatosis has been reported, this was not the case in our patient as she did not fulfill the criteria for the diagnosis of type 1 neurofibromatosis [18].
Histologically, glomus cells appear as round to cuboidal cells with round/oval punched-out nuclei and slightly eosinophilic cytoplasm [15]. Glomangiomas have dilated venous channels and bear a resemblance to venous malformations. They also demonstrate single-to-multiple rows of surrounding cuboidal glomus cells, unlike venous malformations [10,15,19]. The histologic findings in the index patient were largely typical of the above description. Routine laboratory tests are not helpful in the diagnosis of glomangiomas. Ultrasonography and MRI are currently the main tools available for direct imaging of glomus tumors, with high-resolution MRI being shown to be more effective. It can be used to assess tumor borders and differentiate tumor forms based on the dominant cellular pattern, but it is not of clinical significance [20].
Treatment of glomangiomas includes complete surgical excision, which has been reported as the most successful therapy and usually does not result in recurrence. In addition, results of laser therapy (Argon and carbon dioxide) and sclerotherapy have been satisfactory [21,22]. Total excision of all the lesions was done for our patient with a good outcome.
Prognosis is essentially good despite the well-documented clinical features that glomangiomas are a well-known cause of chronic pain in the digits [8]. In addition, on rare occasions, glomangiomas are accompanied by sarcomas to form glomangiosarcoma [8].
Conclusion
Glomangiomas are uncommon and benign tumors of the glomus body. It can be familial; however, most reported cases are sporadic. We reported a case of glomangioma on the lower limb (thigh), which was initially diagnosed as neurofibroma. Clinical diagnosis still remains a challenge which explains the long duration of symptoms to diagnosis time and multiple consultations of physicians before diagnosis. Therefore, an early biopsy of the suspected lesion is essential. The outcome of management is essentially excellent, and it involves modalities such as surgery, laser therapy, and sclerotherapy.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Cutaneous glomangiomas; Benign tumors; Glomus cells
Cite this article
Abimiku PS, Okoro OE, Garba AY, Olarinoye GM, Oseze HU, Magaji D, et al. Cutaneous glomangiomas of the lower limb: A case report. Clin Oncol J. 2022;3(2):1–4.
Copyright
© 2022 Obumneme Emeka Okoro. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).