Barriers in Palliative Care Referrals by Oncology Providers
Meador A;
* Waldron B;
Fiandt K;
-
Meador A: College of Nursing, University of Nebraska Medical Center, NE, USA.
-
* Waldron B: College of Nursing, University of Nebraska Medical Center, NE, USA.
-
Fiandt K: College of Nursing, University of Nebraska Medical Center, NE, USA.
-
Mar 31, 2025 |
-
Volume: 6 |
-
Issue: 1 |
-
Views: 772 |
-
Downloads: 1962 |
Abstract
Cancer is the second leading cause of death globally, with 10 million fatalities in 2020. Despite advancements in treatment, significant gaps exist in holistic care, particularly in Palliative Care (PC). This study evaluated barriers and referral practices among healthcare providers to improve PC access and outcomes for oncology patients. A descriptive survey was conducted among physicians, advanced practice providers, and case managers at a large hospital, gathering qualitative and quantitative data on PC knowledge, referral competencies, and attitudes.
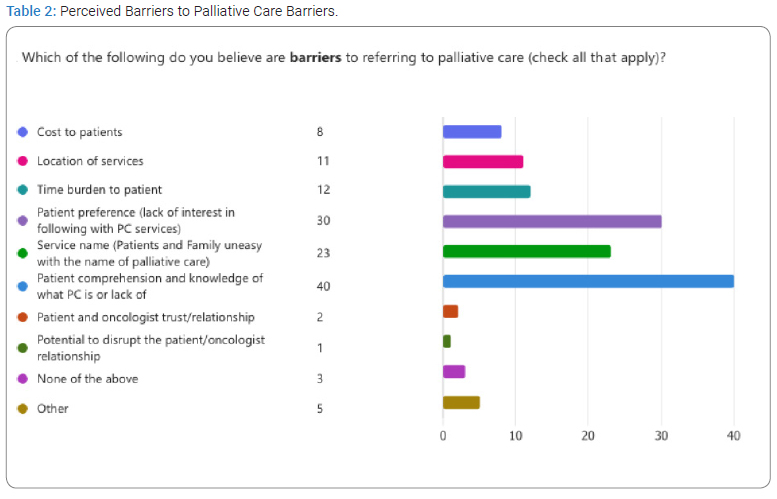
Out of 200 surveyed, 50 responded, with the majority female (n = 46). Respondents included nursing case managers (n = 26), advanced practice providers (n = 13), and physicians (n = 10). Notably, 86% reported no formal PC training during their initial education, although 66% pursued continuing education in PC. While 84% strongly agreed that PC enhances quality of life, only 44% showed a strong interest in further PC education. Barriers to PC referral included patient comprehension (n = 40), patient preference (n = 30), and unfamiliarity with the service name (n = 23).
The survey results revealed a lack of consensus on the timing of PC referrals, despite current guidelines recommending referral at the time of cancer diagnosis. Providers’ comfort in offering comprehensive treatment, goals of curative care, and patient misconceptions about PC were identified as influencing factors. The survey underscored the need to standardize PC referrals at diagnosis to enhance service utilization. Additionally, the findings emphasized the importance of increasing PC education for providers and patients to address the identified barriers and misconceptions. The study suggests that enhancing PC integration into oncology care through standardized referrals and improved education could significantly improve patient outcomes and quality of life.
Introduction
Barriers to PC Referrals by Oncology Providers: Cancer is the second leading cause of death worldwide, with 9.7 million deaths and 20 million cancer cases newly diagnosed in 2022 [1]. As treatment options for cancer have advanced in the last decades, there is considerable room for improvement in holistic treatment options. One area that has shown advances is the development of the concept of PC. PC seeks to improve the quality of life and reduce the disease and symptom burden, with or without curative disease treatment and is particularly beneficial to patients with a cancer diagnosis. However, gaps in practice exist in patient access, utilization of PC services, and delays in timely referral. It is estimated that only 14% of people who would benefit from PC worldwide receive it, demonstrating the expanding need for PC [2].
This project aimed to identify barriers, knowledge gaps, and referral practice challenges in PC for oncology patients, as emphasized by NCCN [4] guidelines that have focused on providing PC to cancer patients despite their stage and diagnosis. Addressing these issues can reduce clinician obstacles, enhance patient outcomes, and promote awareness and acceptance of PC among patients, families, and providers. The survey results will be used to develop a program designed to address provider gaps and increase the likelihood that they will refer patients to PC. To improve PC services, interdisciplinary teamwork, and impact patient outcomes, a baseline survey of involved providers was conducted to assess various domains as they apply to PC.
Review of Literature: PC is designed to improve the quality of life for individuals with life-threatening illnesses by addressing psychological, physical, social, and spiritual needs. The World Health Organization [2] and the National Institute on Aging define PC as a team-based approach that can be provided alongside curative treatments, unlike hospice care, which focuses solely on end-of-life comfort [2,3]. Research indicates that the terminology used to describe PC significantly affects its perception, with terms like “supportive care” being more positively received compared to “PC,” which is often associated with end-of-life care [5].
The integration of PC into active oncology care has been shown to enhance the quality of life, symptom management, patient satisfaction, and survival rates, and it has contributed to reducing healthcare costs and improving patient care experiences [6–9]. Organizations such as the WHO, ASCO, and NCCN advocate for the early integration of PC into standard oncology care [4,10]. Despite its benefits, several barriers hinder PC utilization, including lack of awareness, workforce shortages, inadequate organizational capacity, and misconceptions about PC. These misconceptions often lead to PC being perceived solely as end-of-life care, which limits its utilization [11–13]. Physicians sometimes avoid PC referrals due to fears of diminishing patient hope or trust and lack of clarity about when PC should be introduced [14,15].
Addressing these barriers requires improving education about PC for both patients and providers and establishing standardized referral practices to ensure that the benefits of PC are realized throughout the cancer care continuum [16–18].
Our society emphasizes demands to find cures for cancer and promotes advancing treatments. While many aspects of this innovative, disease-centered approach are necessary, the patient-centered approach allows for improved perception and ability to manage physical and psychological distress [19,20]. While multiple studies have clearly reported the benefits of palliative and patient-centered approaches, the tumor-centered approach continues to be overshadowed. Studies such as those by Slama et al. [21] show how an integrated approach across disciplines toward PC is necessary for improving quality of life, among other patient indicators. Until then, the potential advantages of PC for oncology patients will not be achieved.
Barriers and Current State of PC: The team-based specialty of PC has gained support for its impact on relieving suffering in people with serious illnesses from a variety of professionals in areas of pain, symptom management, and illness support options; barriers and access to PC exist. These barriers have been recognized to occur in five domains: lack of public and professional awareness of PC and its associated benefits; workforce shortages and inadequate training; insufficient organizational capacity and lack of payment programs; inadequate evidence to base safe and effective practice models; as well as lack of regulatory requirements, standards to ensure access and quality [9].
Misconceptions and a lack of understanding of PC can interfere with the utilization and benefits received from PC services. Participation in PC services will increase if proper education about PC is given to patients. Before this education or consultation occurs, PC is often seen as ambiguous. Misinterpretations of its true definition can lead patients and caregivers to associate it solely with dying, end-of-life, hopelessness, dependency, comfort care, and more. PC can be provided alongside treatment and medical interventions. The option for this simultaneous care is often unknown. Fear and avoidance are attitudes that stem from this lack of knowledge [11–13]. Many of these misconceptions were pre-consultation.
Combating viewpoints on physicians’ use of PC versus supportive care exists. In one study, oncologists reported that a name change and use of supportive care over PC did not change referral patterns and rates [22]. However, work by Hui et al. [23] showed a preference by oncologists to use supportive care over PC when referring patients. These alternative viewpoints bring attention to the challenges, varying communication skills, and strategies by physicians that may be impacting referral rates and practices.
Attitudes and perceptions held by physicians can impact the delivery of care and services to patients, regarding these concepts as important aspects to evaluate when considering PC for oncology patients. Cultural and physician-held beliefs and attitudes toward PC can have positive and negative implications. Physicians have a positive attitude toward PC in general, as well as toward specialists, clinics, and services that provide care to patients [22,24,25]. However, there are identified misconceptions, blurred comprehension, and poor understanding of PC and whether it should be regarded as “supportive care,” “end-of-lifecare,” or “hospice.” The lack of one definition, poor comprehension, and associated misunderstandings affect providers and subsequent barriers to patient service delivery [26–29]. With these blurred views, there are varying opinions as to when PC should start, as there is no consensus, resulting in fluctuating attitudes and practices. Various beliefs held by providers are that PC should start at diagnosis, or congruent with cancer treatment, or after treatment options run out [24,27,30,31].
The existence of negative attitudes and perceptions of referring patients to PC exist and have been documented in a few studies. Unfortunately, the consequences reported by providers are that they are fearful and afraid of failing their patients when providing a referral to PC [31]. Many providers perceive that their patients and families will lose hope or trust in them to care for them after a diagnosis of cancer and through treatment. They perceive that their patients will have a negative attitude toward them and how they deliver care and services. Other preconceived notions are that providers believe that their patients and families will not understand PC, and they, for referral, are concerned that it means it is end-of-life or impending death [14,15,26].
Providers experience challenges within their organization of supporting or providing PC services. Lack of specialty PC services, providers, and clinics impact the delivery of care to patients. Furthermore, poor access, utilization, limited time, inadequate communication between specialists, and insignificant reimbursement for services have been reported as system issues by physicians [14,27,31,32] within the large cultural framing of PC.
The concept of referral to PC by providers is not well defined or understood, building on misconceptions. Preconceived attitudes, knowledge, skills, and capacity of providers to overcome barriers impact referrals to PC for cancer patients. Of note from provider perspectives, referrals to PC, unfortunately, can happen late in the disease process [16], even with the recognized importance and benefits of PC to patients held by providers [17,18,28]. As reported by physicians, referrals to PC are typically more for physical and disease-related characteristics, with the most common being pain management rather than psychological or social concerns [27,30,33].
Challenges reported by doctors, in addition to a lack of support staff and clinics for providing PC services, are a challenge in delivering care to chronically complex patients. Many providers reported they have patients who either have no symptoms that require specialty care or are unwell and rapidly deteriorate after diagnosis [17,33]. Many providers find themselves delivering necessary additional services to patients along the cancer continuum, such as addressing pain, nausea, and other physical needs. They feel they can treat these symptoms within their scope of practice. However, many articles touched on aspects that providers face challenges in when to refer patients, or which providers are responsible for aspects of patient care, as there are no set models for delivery of care [15,31–34].
Materials and Methods
While PC is needed beyond outpatient oncology, the current team primarily serves the cancer center. The study gathered self-reported data through an electronic survey sent to physicians, advanced practice providers, and case managers who refer oncology patients to the outpatient PC service. These participants are from departments such as general oncology, hematology and bone marrow transplant, radiology oncology, and surgical oncology, each encompassing various specialties. This DNP project is a descriptive study of providers’ perceptions of PC, detailed in (Appendix B).
The Microsoft Forms survey was distributed via institutional email and remained open for four weeks, with a reminder sent halfway through. The survey allowed easy access to results and export to Excel for analysis. It covered various domains, including baseline PC knowledge, referral competencies, and provider attitudes. Survey links were sent anonymously to protect participant identities, and demographic data collected included licensure type, specialty, years of oncology practice, PC experience, education, and training. Survey questions were adapted from established methods, ensuring only face validity was assessed, as reliability was not calculated.
Microsoft Forms facilitated descriptive analysis by transcribing qualitative responses and one open-ended quantitative question to identify trends and rankings at the survey’s conclusion.
Demographic and employment data highlighted participants’ specialties and backgrounds, revealing their involvement patterns. The summarized data and rankings were shared with the director of PC and disseminated within the department. The survey aimed to enhance team collaboration, increase service utilization, reduce barriers, and improve referral strategies to the outpatient PC clinic. While further research can be conducted post-analysis, no substantial qualitative data required statistical input, and all collected responses were retained for analysis purposes.
Confidentiality and anonymity were maintained throughout the study, with data securely stored and accessible only to authorized investigators. No conflicts of interest were present, and survey results were shared post-analysis to potentially enhance PC utilization. Contact information and IRB details were provided for participant inquiries.
Results
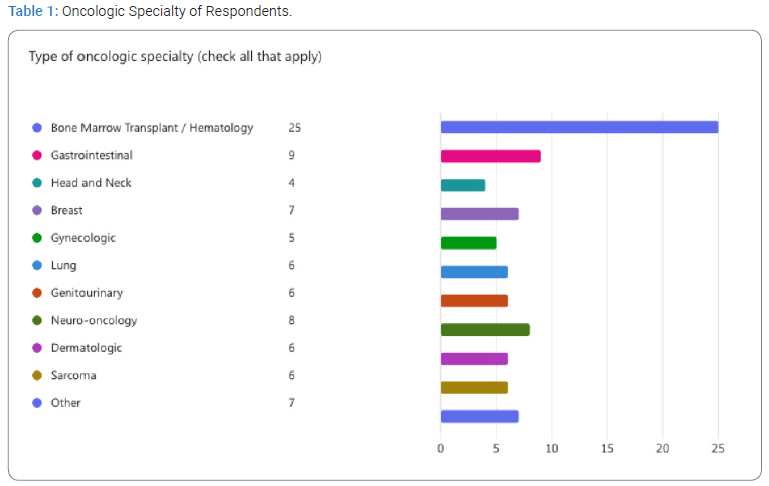
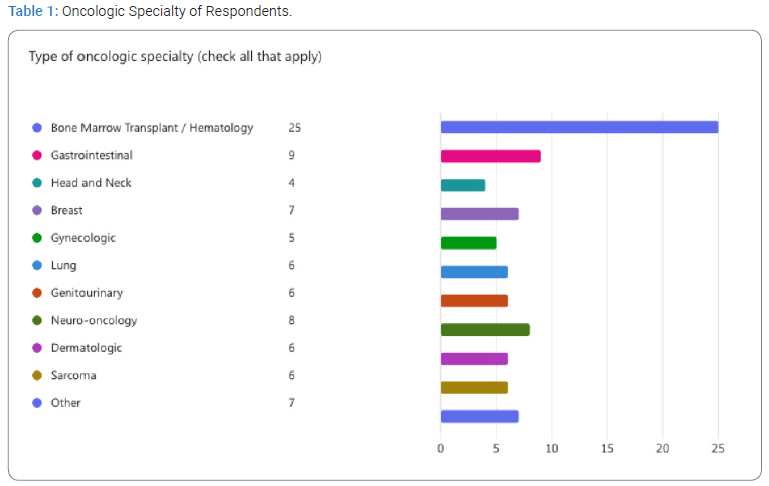
Participants: During the survey period, 50 respondents out of 200 surveyed physicians, advanced practice providers, and case managers returned usable surveys from the main campus location of the hospital system. Demographic details of respondents were female (n = 46) versus male (n = 4) participants, with selected professional roles as follows: nursing case managers (n = 26), APPs (n = 13), physicians (n = 10), and others (n = 1). Specialty demographics of respondents are dispersed throughout General Oncology (n = 21), Bone Marrow Transplant/Hematology (n = 16), Other (n = 6), Surgical Oncology (n = 4), and then Radiation Oncology (n = 3). Specialty department designation by profession is available as a select all that apply, presented in (Table 1). The other selection criteria allowed for input by the respondent in which some responses for others were written one time each, as follows: all the above: pancreas, pediatric, Leukemia/Benign Heme Hematology/oncology Fellow, and 50+-year-old geriatric cancer patients.
Sixteen participants had over 20 years of experience, and the rest had less experience.
Importantly, 43 respondents reported not receiving formal training in PC during residency, graduate school, etc.; however, 33 respondents have pursued continuing education content in areas of PC.
Perceptions of PC Results: Respondents were asked to rate statements with ratings ranging from strongly disagree, disagree, neutral, agree to strongly agree to a series of questions regarding knowledge, skills, and attitudes surrounding PC and referral situations for oncology patients.
Significant responses were that 42 participants responded with strongly agree regarding notions that PC benefits include enhanced quality of life for patients and families. When asked if they were interested in increasing their knowledge of PC, 22 responded strongly agreeing, which would include the potential of attendance at a seminar or workshop (Appendix B, question 9).
When asked when PC services were appropriate for various situations for oncology patients, 24 respondents either strongly disagreed or disagreed with the notion that patients are not appropriate to PC services if they are no longer receiving active treatment due to a cured cancer state. While providers believed in the benefits of PC, eight respondents disagreed with a referral to PC if patients were receiving active cancer treatment for curative intent (Appendix B, questions 10 and 11).
Additional respondents noted additional barriers to referrals to PC. Seven providers agree, or strongly agree, with the statement that they would not make a referral because they “have the capacity to provide PC services to their patients rather than make a referral.” In asking providers to describe their level of comfort, three strongly disagree, and 17 disagree that they would feel comfortable managing depression and/or anxiety for their patients; eight disagree, and three strongly disagree that they are comfortable discussing advance care planning with their patients (Appendix A, question12).
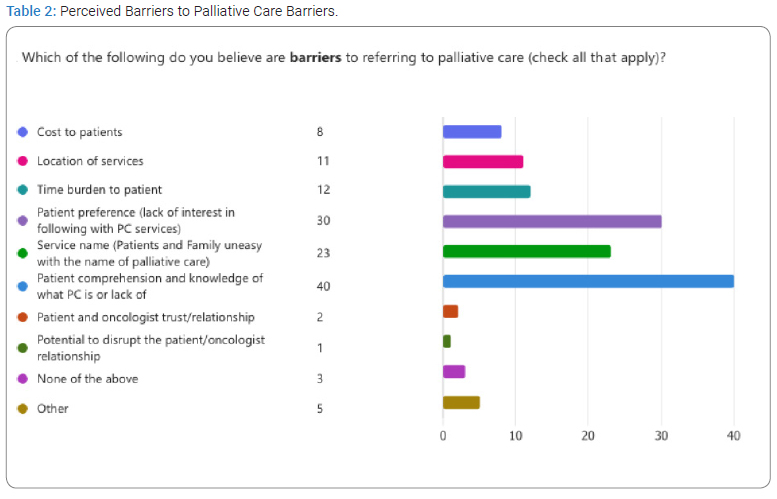
Barriers: Respondents were asked to select all that apply when prompted to identify which of the following were barriers to PC: cost to patients, location of services, time burden to the patient, patient preference, service name, patient comprehension, patient/provider trust, potential to disrupt the oncologist/patient relationship, none of the above, and/or other.
The greatest barrier identified is that patients lack comprehension of what PC is (n = 40), followed by patient preference or lack of interest in PC services (n = 30), and the third largest selected barrier was that the service name may be unfamiliar to patients and families (n = 23). (Table 2) displays the distribution of the barriers identified. Few respondents selected other and wrote in items as follows: “Getting the physicians that we work with to agree to the referral’; “Patients or families unwilling to stop anti-cancer therapy”; “Lack of understanding of PC from the provider”; “physicians not discussing with pts”; and lastly, “Sometimes the oncologist does not want to involve PC.”
Major Themes in Open-Ended Responses: At the end of the survey, 26 participants provided open-ended responses about their PC experience and the referral process, revealing several key themes. Many respondents recognized PC as a valuable resource and expressed their intention to continue making referrals. Providers reiterated common barriers and concerns brought forth by patients, noting that patients often fear PC due to confusion about its purpose and the distinction between palliative and hospice care, leading to anxiety and refusal of consultations despite provider discussions. Additionally, there was a strong call for enhanced education for PC providers and patients. Participants suggested introducing PC during diagnosis to improve awareness and comfort throughout a patient’s illness trajectory. They also highlighted coordination issues and a lack of available PC providers as obstacles to effective referrals.
Discussion
The survey intended to determine oncology providers’ knowledge and attitudes regarding PC, their comfort in having conversations surrounding PC, and uncovering barriers to patient referrals.
Survey results present a gender bias in the total female and male participants. This representation demonstrates evidence of a female-dominated healthcare workforce, more particularly in nursing roles, such as nurse case manager representations [35]. Demographic findings from the survey reinforce the longevity of providers within oncology specialties, as well as the lack of formal education in PC. However, providers do not show a lack of interest in the pursuit of continuing education or enhanced learning opportunities. There has been growing support for PC, not just for implementation and utilization by patients and families but also by the healthcare community to improve knowledge and comprehension and increase education and training opportunities across professions and specialties [36]. Findings from the survey reinforce the evidence supporting the utilization and services of PC as perceived by the benefits to patients and families.
Furthermore, providers strongly believe that PC benefits include enhanced quality of life. However, it is evident that providers and patients have issues with navigating and defining PC, determining when patients are appropriate for referral, and getting providers, patients, and families to buy in with PC services. The study results reinforce underlying societal comprehension issues of defining PC, differentiating PC from hospice, and encouraging patients and families to be interested and engaged in PC services, even during active cancer treatment [7]. Language and comprehension of PC across provider and patient populations are highlighted barriers and perceived limitations to the uptake of services, as provided by this research and in the current literature. Current NCCN guidelines recommend PC referrals at the time of cancer diagnosis. Survey results show that while many providers agree that PC services are suitable for newly diagnosed patients, there is no consensus on when to initiate referrals. Factors influencing referral timing include providers’ comfort with comprehensive treatment, goals of curative care, and patients’ understanding of PC services. Implementing a standard practice of referring to PC upon diagnosis could enhance access and utilization of these services. The survey also revealed that providers view patients’ lack of knowledge and interest in PC as key barriers to successful referrals, highlighting a gap in patient education and societal perceptions.
Survey participants were positively interested in increasing knowledge and education around PC and associated services for patients. This finding is congruent with research that supports the growth, implementation, and integration of PC into various organizations, educational programs, and continuing education opportunities for providers and case managers. Results show positive perceptions of PC; however, underlying misconceptions persist with the differentiation of PC versus hospice or end-of-life care, evidenced by statements provided in the survey and the literature evaluating patient and family perceptions. This stigma must be replaced with factual education and the promotion of the multitude of physical, psychosocial, and spiritual, among many other benefits PC services can offer a patient and their families. Shifting the language will decrease anxiety and apprehension around the subject, leading to a more open approach.
Limitations
The current study has limitations, including its focus on a single facility, potential gender bias, and a concentration on outpatient PC services exclusively for oncology patients. While the results reflect healthcare personnel’s views, they may not be generalizable to other institutions.
Additionally, there is a potential bias toward positive perceptions of PC since respondents took the time to participate in the survey. The response rate was lower than ideal but expected due to the busy schedules of targeted participants. Further research is needed to understand patients’ and families’ perceptions of PC, the referral process, and services provided by PC providers.
Additionally, analysis of the impact of nursing roles, such as nurse practitioners and case managers, on PC is warranted. The NCCN recommends that all cancer patients receive a PC consult; however, the hospital’s current utilization of these services remains unclear, and referrals are assumed to be underutilized. By administering the proposed survey, barriers related to knowledge, skills, and attitudes can be identified and addressed, facilitating improved PC services for those in need and providing a foundation for necessary changes.
Conclusions
Overall, findings in this survey reflected previous research findings and common misconceptions surrounding PC. All participants supported PC and agreed its benefits include enhanced quality of life for patients and families, supported by open-response claims that many providers routinely refer and are comfortable doing so. Survey results reflect the potential impact that case managers may have in collaborating with providers in influencing PC referrals for patients.
The current research findings emphasize the importance of PC among healthcare professionals and contribute evidence to improve and expand PC referral processes and services. There is a consistent interest in further education and training to enhance service delivery and improve communication methods for better patient care. This survey highlights the existing barriers faced by both patients and providers in referring oncology patients to outpatient services. Additionally, this research offers a deeper analysis of PC by incorporating the perspectives of nurses, advanced practice providers, and case managers.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- American Cancer Society. The global cancer burden [Internet]. Georgia: American Cancer Society; 2020.
- World Health Organization. Palliative care[Internet]. Geneva: WHO; 2020.
- National Institute on Aging. What are palliative care and hospice care? [Internet]. USA: National Institute on Aging; 2021.
- National Comprehensive Cancer Network. Palliative care [Internet]. NCCN; 2023.
- Maciasz RM, Arnold RM, Chu E, Park SY, White DB, Vater LB, et al. Does it matter what you call it? A randomized trial of language used to describe palliative care services. Support Care Cancer. 2013;21(12):3411–3419.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302(7):741–749.
- Fulton JJ, LeBlanc TW, Cutson TM, Porter Starr KN, Kamal A, Ramos K, et al. Integrated outpatient palliative care for patients with advanced cancer: A systematic review and meta-analysis. Palliative Medicine. 2019;33(2):123–134.
- Temel JS, Greer JA, Admane S, Gallagher ER, Jackson VA, Lynch TJ, et al. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non–small-cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol. 2011;29(17):2319–2326.
- Meier DE, Back AL, Berman A, Block SD, Corrigan JM, Morrison RS. A national strategy for palliative care. Health Affairs. 2017;36(7):1265–1273.
- Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA, Basch EM, et al. American society of clinical oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J Clin Oncol. 2012;30(8):880–887.
- Collins A, McLachlan SA, Philip J. Initial perceptions of palliative care: An exploratory qualitative study of patients with advanced cancer and their family caregivers. Palliative Medicine. 2017;31(9):825–832.
- Gemmell R, Halley A, Stevens AM, Allam A, Perkins M, Ethell M, et al. Palliative care for patients around the time of haematopoietic stem cell transplant: a qualitative study of patients’ perceptions and experiences of unmet need and attitudes towards palliative care involvement. Support Care Cancer. 2022;30(3):2253–2261.
- Hannon B, Swami N, Pope A, Leighl N, Rodin G, Krzyzanowska M, et al. Early palliative care and its role in oncology: A qualitative study. The Oncologist. 2016;21(11):1387–1395.
- Cripe JC, Kathryn AM, Kuroki LK, Wan L, Hagemann AR, Fuh KC, et al. Gynecologic oncologists’ perceptions of palliative care and associated barriers: A survey of the society of gynecologic oncology. Gynecol Obstet Invest. 2018;84(1):50–55.
- Pini S, Hackett J, Taylor S, Bekker HL, Kite S, Bennett MI, et al. Patient and professional experiences of palliative care referral discussions from cancer services: A qualitative interview study. Eur J Cancer Care (Engl). 2021;30(1):e13340.
- Wentlandt K, Krzyzanowska MK, Swami N, Rodin GM, Le LW, Zimmermann C. Referral practices of oncologists to specialized palliative care. J Clin Oncol. 2012;30(35):4380–4386.
- Feld E, Singhi EK, Phillips S, Huang LC, Shyr Y, Horn L. Palliative care referrals for advanced non– small-cell lung cancer (NSCLC): Patient and provider attitudes and practices. Clin Lung Cancer. 2019;20(3):e291–e298.
- Kruser TJ, Kruser JM, Gross JP, Moran M, Kaiser K, Szmuilowicz E, et al. Medical oncologist perspectives on palliative care reveal physician-centered barriers to early integration. Ann Palliat Med. 2020;9(5):2800–2808.
- Hjermstad MJ, Hamfjord J, Aass N, Dajani O, Lundeby T, Wester T, et al. Using Process Indicators to Monitor Documentation of Patient-Centred Variables in an Integrated Oncology and Palliative Care Pathway-Results from a Cluster Randomized Trial. Cancers. 2021;13(9):2194.
- Tsvitman I, Castel OC, Dagan E. The association between perceived patient-centered care and symptoms experienced by patients undergoing anti-cancer treatment. Support Care Cancer. 2021; 29(11):6279–6287.
- Slama O, Pochop L, Sedo J, Svancara J, Sedova P, Svetlakova L, et al. Effects of early and systematic integration of specialist palliative care in patients with advanced cancer: Randomized controlled trial PALINT. J Palliat Med. 2020;23(12):1586–1593.
- Rhondali W, Burt S, Wittenberg-Lyles E, Bruera E, Dalal S. Medical oncologists’ perception of palliative care programs and the impact of name change to supportive care on communication with patients during the referral process. A qualitative study. Palliat Support Care. 2013;11(5):397–404.
- Hui D, Park M, Liu D, Reddy A, Dalal S, Bruera E. Attitudes and beliefs toward supportive and palliative care referral among hematologic and solid tumor oncology specialists. The Oncologist. 2015;20(11):1326–1332.
- Agne JL, Bertino EM, Grogan M, Benedict J, Janse S, Naughton M, et al. Too many appointments: assessing provider and nursing perception of barriers to referral for outpatient palliative care. Palliat Med Rep. 2021;2(1):137–145.
- Wong A, Reddy A, Williams JL, Wu J, Liu D, Bruera E, et al. ReCAP: Attitudes, beliefs, and awareness of graduate medical education trainees regarding Palliative Care at a Comprehensive Cancer Center. J Oncol Pract. 2016;12(2):149–150; e127–e137.
- Sarradon-Eck A, Besle S, Troian J, Capodano G, Mancini J. Understanding the barriers to introducing early palliative care for patients with advanced cancer: A qualitative study. J Palliat Med. 2019;22(5):508–516.
- Schenker Y, Crowley-Matoka M, Dohan D, Rabow MW, Smith CB, White DB, et al. Oncologist factors that influence referrals to subspecialty palliative care clinics. J Oncol Pract. 2014;10(2):e37–e44.
- Tarberg AS, Thronaes M, Landstad BJ, Kvangarsnes M, Hole T. Physicians’ perceptions of patient participation and the involvement of family caregivers in the palliative care pathway. Health Expect. 2022;25(4):1945–1953.
- Wallerstedt B, Benzein E, Schildmeijer K, Sandgren A. What is palliative care? Perceptions of healthcare professionals. Scand J Caring Sci. 2019;33(1):77–84.
- Barni S, Maltoni M, Tuveri G, Pronzato P, Cortesi E, Massidda B, et al. Attitude of Italian medical oncologists toward palliative care for patients with advanced cancer: Results of the SIO project. Support Care Cancer. 2010;19(3):381–389.
- Ward AM, Agar M, Koczwara B. Collaborating or co-existing: a survey of attitudes of medical oncologists toward specialist palliative care. Palliative Medicine. 2009;23(8):698–707.
- Horlait M, Chambaere K, Pardon K, Deliens L, Van Belle S. What are the barriers faced by medical oncologists in initiating discussion of palliative care? A qualitative study in Flanders, Belgium. Support Care Cancer. 2016;24(9):3873–3881.
- Johnson CE, Girgis A, Paul CL, Currow DC. Cancer specialists’ palliative care referral practices and perceptions: results of a national survey. Palliative Medicine. 2008;22(1):51–57.
- Brockway JP, Murari K, Rosenberg A, Saigh O, Press MJ, Lin JJ. Differences in primary care providers’ and oncologists’ views on communication and coordination of care during active treatment of patients with cancer and comorbidities. International Journal of Care Coordination. 2019;22(2):51–57.
- United States Census Bureau. Explore Census Data [Internet]. Maryland: United States Census Bureau; 2023.
- Kamal AH, Wolf SP, Troy J, Leff V, Dahlin C, Rotella JD, et al. Policy changes key to promoting sustainability and growth of the specialty palliative care workforce. Health Aff (Millwood). 2019;38(6):910–918.
Keywords
Palliative care; Oncology; Barriers; Education
Cite this article
Meador A, Waldron B, Fiandt K. Barriers in Palliative Care Referrals by Oncology Providers. Clin Oncol J. 2025;6(1):1–7.
Copyright
© 2025 Waldron B. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).