Abstract
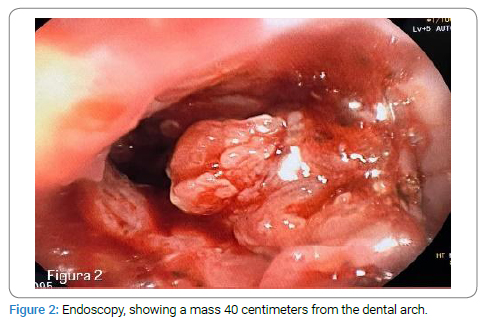
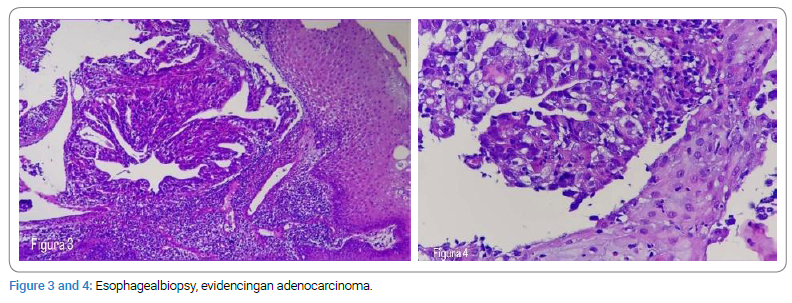
The case of a patient is 35-year-old patient with no known history of smoking, alcoholism, obesity, or gastroesophageal reflux disease who presented to the emergency room with a history of dysphagia for six months and abdominal pain located in the epigastric region. Secondary to dysphagia progressing from solid to liquid food, decreased food intake, and a 70-pound weight loss. An endoscopy was performed, evidencing a mass of 40 centimeters from the dental arch. A biopsy was taken, reporting an adenocarcinoma of the esophagus and gastroesophageal junction.
Introduction
The esophagogastric junction is particularly vulnerable to damage from gastric acid and subsequently has a higher risk of malignant transformation. The incidence of cancer of the esophagogastric junction is increasing, and because in early stages, the patient may remain asymptomatic, it is diagnosed in advanced stages of the disease [1]. Tumors of the esophagogastric junction are generally those that compromise this junction and that originate in the distal esophagus or in the stomach in its proximal region. Multiple risk factors are associated with this cancer, such as smoking, overweight and obesity, alcoholism, and gastroesophageal reflux disease. The course of the disease is considered to be lethal. Since the symptoms that are presented are not specific to the disease, so the moment the diagnosis is made, the patient is in advanced stages [2].
Case Presentation
The patient is 35-year-old patient with no known history of smoking, alcoholism, obesity, or gastroesophageal reflux disease who presented to the emergency room with a history of dysphagia for six months and abdominal pain located in the epigastric region reported that around six months ago she began with dysphagia localized in the sternum region, with solid foods and later progressed to solid and liquid foods. The dysphagia is accompanied by abdominal pain of progressive onset, located in the epigastrium, “cramping” type, intensity 10/10 on the pain scale, does not irradiate, and is not completely relieved with an analgesic. She decides to see a private doctor who prescribes a proton pump inhibitor, but there is no improvement. During the last four months, he reported a weight loss of approximately 70 pounds, which is why he decided to consult another private doctor again, but they did not find a diagnosis, and they decided to refer him to this center for “anemia.”
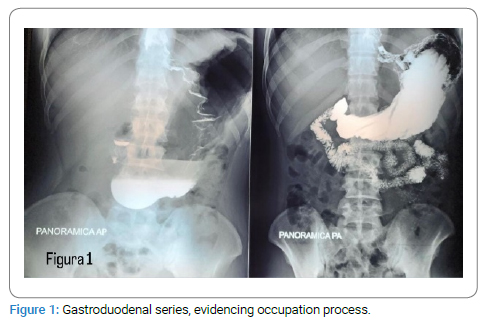
Upon admission, complete hematology was requested with the following results: white blood cells: 32.53*10^3, neutrophils: 91.80%, hemoglobin: 11.20 g/dL, and platelets at 312,000. In addition, a gastroduodenal series was requested, showing dilation of the distal third of the esophagus, secondary to the presence of a polypoid mass at the level of the gastroesophageal junction, with thick and thin thickening, which forms an irregular stenosis; as well as their regularity and rigidity of the cardia and gastric fundus (Figure 1).
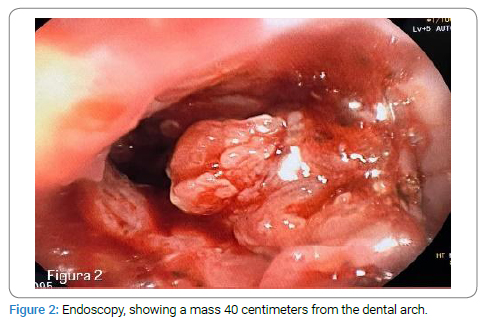
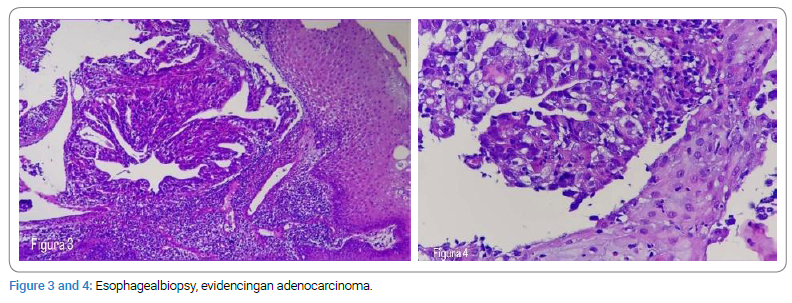
Due to fluoroscopic findings, he presented to gastroenterology, and an endoscopy was performed, where a mass was found in the esophagus 40 centimeters from the dental arch, extending to the gastroesophageal junction and gastric fundus (Figure 2). A biopsy was taken, and a pathology report was received, evidencing a large cell neoplasm with a glandular, papillary, and solid growth pattern. Showing cells with large, pleomorphic nuclei, coarse granular chromatin, prominent nucleoli, and extensive eosinophilic cytoplasm (Figure 3,Figure 4). In conclusion, an adenocarcinoma of the gastroesophageal junction and distal esophagus. He presented to the oncology department for further monitoring and treatment.
Discussion
Most risk factors associated with young patients consist of obesity, poor nutrition, and human papillomavirus infection. Being very overweight and having too much body fat can increase a person’s risk of developing esophageal adenocarcinoma. A diet low in fruits and vegetables and certain vitamins and minerals can increase a person’s risk of developing esophageal cancer [2]. The esophagogastric junction is the site where the esophagus joins the cardia of the stomach. Endoscopically, it corresponds to the most proximal site of the gastric folds. The incidence of adenocarcinoma of the esophagogastric junction has been increasing worldwide, and the incidence patterns of esophageal adenocarcinoma are now more frequent than squamous cell cancer [3].
Among the factors that can predispose a patient to cancer of the esophagogastric junction is associated with advanced age, sex, alcoholism, smoking, and esophagogastric reflux disease. In our case, it can be noted that the patient did not have almost any risk factor associated with the development of this type of cancer, being the male sex the only associate. In our case, we found that the patient’s age is 35 years. Generally, the risk of developing esophagogastric junction cancer increases with age, a pattern found worldwide. Tumors of the esophagogastric junction are defined as those that originate from the esophagogastric junction or the cardia in the first 5 centimeters, extending to the esophagus [4].
The clinical presentation of the patient depends on the progress of the disease; In early stages, the patient may be asymptomatic or present retrosternal pain or discomfort, and in late stages, they usually have a systemic presentation: weight loss, dyspepsia, dysphagia, hematemesis, melena, and fatigue [5]. Based on the endoscopic findings, we consider the characteristic location of the esophagogastric junction tumors and the course of the patient’s disease to be in the late stages due to the presentation of systemic symptoms, as mentioned above.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Adenocarcinoma; Esophagogastric junction; Swallowing disorders
Cite this article
Urrutia MJ, Hernández KG, Rodas LA, Ramírez JR, Revolorio DO. Esophagogastric Junction cancer in young patient: a case report. Clin Oncol J. 2023;4(1):1–3.
Copyright
© 2023 Urrutia MJ. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).