Hepatic Actinomycosis Mimics Malignancy
* Seval Akay;
Özamrak BG;
Arici Z;
Ünal OU;
-
* Seval Akay: Department of Medical Oncology, UHS Tepecik Education and Research Hospital, İzmir, Turkey.
-
Özamrak BG: Department of Pathology, UHS Tepecik Education and Research Hospital, İzmir, Turkey.
-
Arici Z: Department of Internal Medicine, UHS Tepecik Education and Research Hospital, İzmir, Turkey.
-
Ünal OU: Department of Medical Oncology, UHS Tepecik Education and Research Hospital, İzmir, Turkey.
-
Jun 26, 2023 |
-
Volume: 4 |
-
Issue: 1 |
-
Views: 2226 |
-
Downloads: 1694 |
Abstract
Hepatic Actinomycosis (HA) is a rare actinomycosis that sometimes confuses with malignancy. Hepatic involvement has been reported in only 5% of actinomycosis cases and is usually facilitated by a history of abdominal surgery, foreign body, pancreatitis, or pancreatic cyst drainage.
We present here a 41-year-old man, a cattle breeder, with no history of surgery, smoking, alcohol, or chronic diseases who complains about tiredness and night sweats. We investigated malignancy because of a hepatic mass on Computerized Tomography (CT) scan that seems as a metastasis. During a hepatic biopsy intervention, he was diagnosed with HA when typical sulfur granules were drained. HA can be misdiagnosed as malignancy, tuberculosis, or other chronic infections. He recovered well with penicillin.
Abbreviations
AFP: Alpha Fetoprotein; CEA: Carcioembriogenic Antigen; CRP: C-Reactive Protein; CT: Computerized Tomography; HA: Hepatic Actinomycosis; Hb: Hemoglobin; USG: Ultrasound
Introduction
Actinomycetes is a rare causative agent of suppurative and granulomatous inflammation that is found in normal oral flora and the lower gastrointestinal tract [1–3]. It grows radially with well-developed branching hyphae. Typical “sulfur granules” form leaky, draining sinuses. This type of infection can occur in thoracic, abdominopelvic, and central regions, mostly in the oral and cervicofacial regions [4]. Although it usually causes chronic infections, it can also cause disseminated diseases. In the case of reports, Actinomycosis was not considered as the initial diagnosis, and the cases were diagnosed on further investigations that show macroscopically typical sulfur granules of Actinomyces or microscopically with central necrotic appearance with microfilaments, even sometimes misdiagnosed as malignancy [5].
There are no comprehensive studies on hepatic Actinomycosis, which are extremely rare. When the case reports were evaluated, most of the cases were reported from Asian countries, and nonspecific complaints such as abdominal pain, weight loss, fever, and night sweats were described mostly in immunocompetent (92%) individuals as an exclusion of other infections or malignancies [6]. This rare infection is frequently observed in men (three times higher than women) aged 20 and 60, with the highest occurrence happening in the age range of 40 years–50 years [7].
Case Presentation
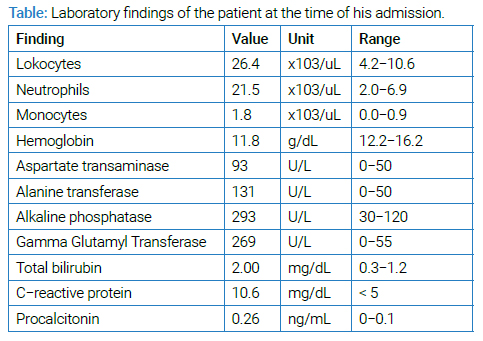
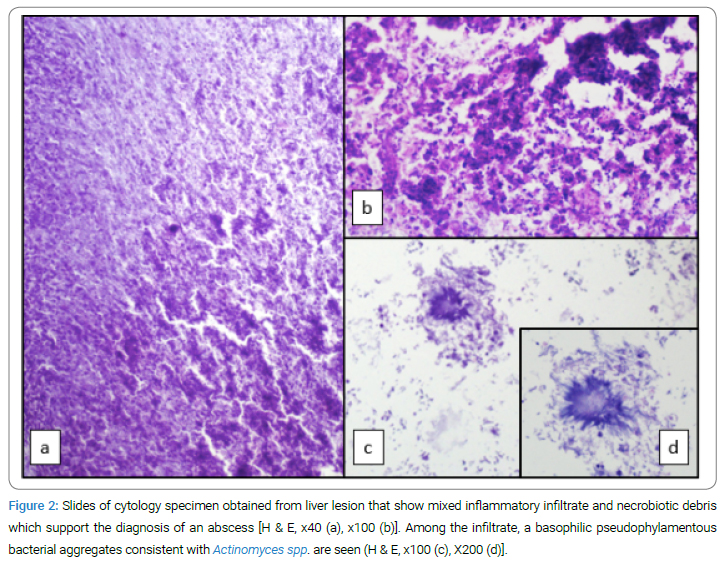
A 41-year-old man, a cattle breeder with no known history of any disease or surgery, presented complaints of fatigue and sweating, which worsened in the last two weeks. Two months ago, he weighed 6 kg more than his current weight. He had no history of smoking, alcohol, or drug abuse. Physical examination revealed no abnormalities except hepatomegaly. Laboratory tests are shown in (Table). The serum tumor marker values (AFP, CEA, beta Hcg, CA 15-3, and CA 19-9) were within normal limits. Hepatitis B, hepatitis C, and human immunodeficiency virus antibodies were negative. Brucellosis was ruled out by testing negative antibodies. Unfortunately, due to a liver mass that was found on ultrasound, he was transferred to our oncology department with a malignancy of an unknown primary site.
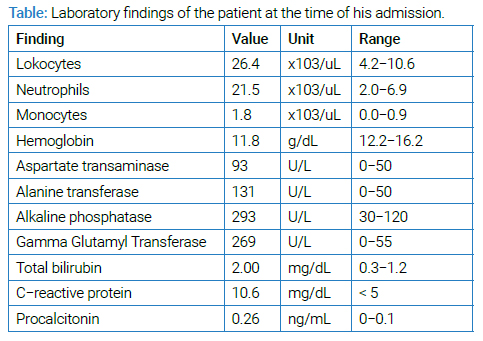
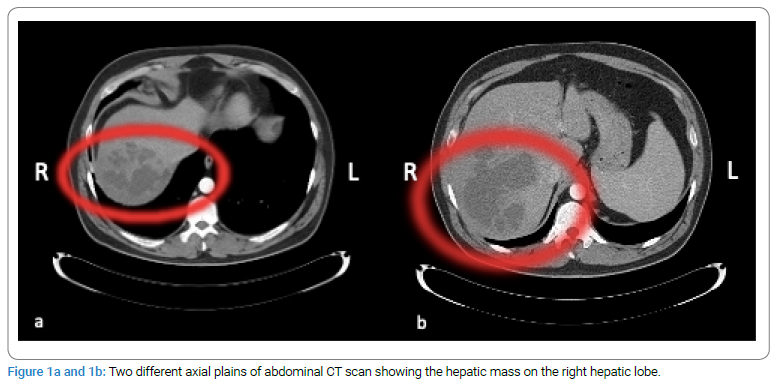
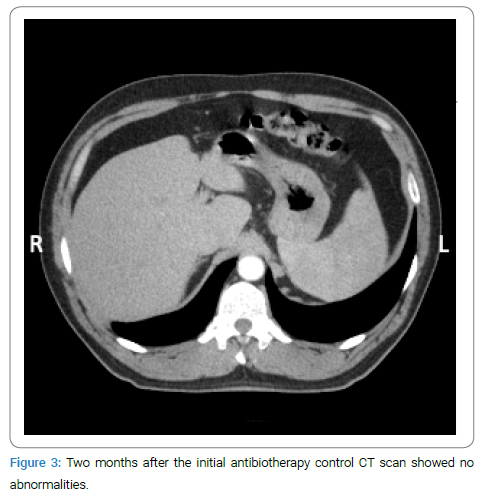
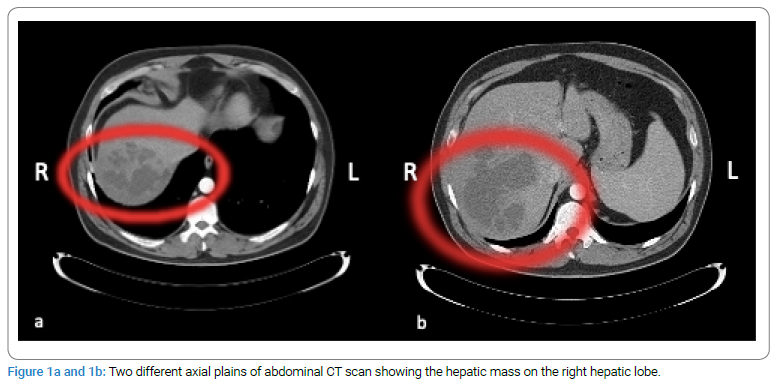
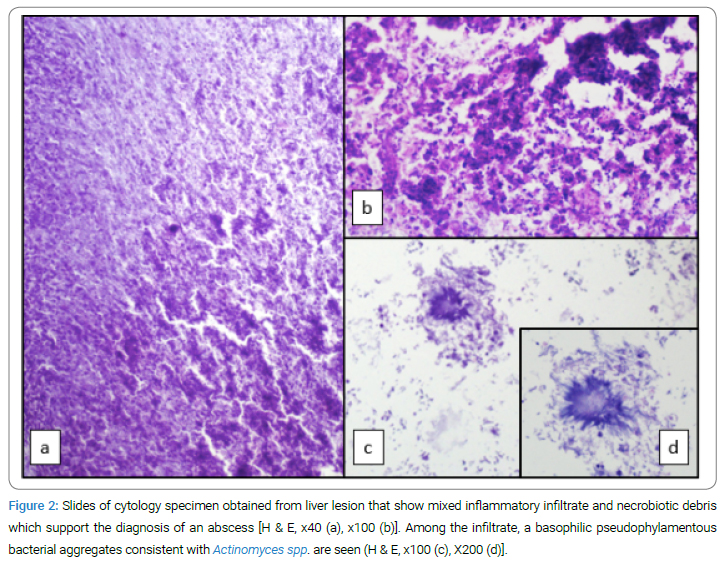
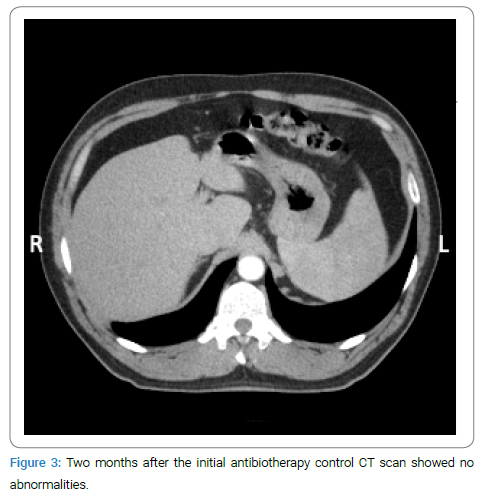
A contrast-enhanced CT scan showed a 13 cm x 12 cm mass localized at the junction of hepatic segments 7 and 8 with an indistinct outer border and large cystic areas (Figure 1). USG-guided liver biopsy was performed with suspicion of malignancy. An abscess was detected during the biopsy. A drainage catheter was inserted, and yellowish granules were drained macroscopically. Under the light microscopic evaluation, polymorphonuclear leukocytes and Gram-positive cocci were observed. Pathologic examination revealed Actinomyces (Figure 2). The patient was treated with cefoperazone/sulbactam 1gm twice a day, parenterally. No mass image was detected on ultrasound which was performed on day 20 of the anti-biotherapy, and the drainage catheter was withdrawn with no discharge through it. Though, CRP and transaminases also returned to normal. Ampicillin/sulbactam 500/250 mg was given orally for six months. On the second month of the anti-biotherapy, CT imaging of the liver showed no abnormalities (Figure 3). The patient is still asymptomatic for 36 months.
Discussion
HA is an extremely rare liver infection; even the exact prevalence is not defined regionally. Abdominal localized infections of Actinomyces occur in 20% of cases and are most commonly localized in the ileocecal region [8,9]. Actinomyces can cause chronic abscesses, especially in situations where the integrity of the gastrointestinal mucosa is compromised, such as through trauma or surgery [10]. Abdominal surgery is the leading condition implicating HA infection, followed by a foreign body, diabetes mellitus, smoking, hypertension, and alcohol use in order of frequency [6]. The hard wall structure around the abscesses gives the perception of a tumor on imaging [11]. However, in a case report, a patient who underwent a Whipple procedure for a pancreatic mass that was radiologically diagnosed as malignant was histopathologically diagnosed with actinomycosis [12].
Gram staining, culture, and histological examination can be used in the differential diagnosis of actinomycosis. Finding yellow-green-colored sulfur granules in the abscess aspirate is easily diagnostic. However, yellowish sulfur granules can also be seen in other infections, such as nocardiosis, although Gram-positive filamentous branching is highly suggestive of actinomycosis [13].
For diagnosing actinomycosis, examining a Gram stain of pus or the infected tissue is more sensitive than a culture test, as it deserves anaerobic conditions, quick take to the laboratory, and prolonged time to reproduction [14]. 16S rRNA sequencing and PCR analysis can also be used to identify Actinomycetes [14]. Actinomyces spp. are found in cattle’s normal gastrointestinal tract flora [15]. However, occupational exposure is a matter of concern. The cutaneous form of actinomycosis was also reported in a cattle breeder [16].
Hepatic actinomycosis can be quite difficult to recognize clinically. Patients may present with nonspecific complaints such as fever, weight loss, malaise, and abdominal pain. Although laboratory findings are variable, CRP elevation, leukocytosis, and alkaline phosphatase elevation may be observed as in any inflammatory condition resulting in systemic findings. Abscess formation may not appear directly on imaging, and the appearance may be deceptive in terms of metastasis. In approximately two-thirds of cases, a right lobe lesion of the liver is observed, while a solitary lesion is present in approximately two-thirds of cases [6,17]. Involvement of the liver may occur through the adjacent organ or the blood [9].
The spectrum of infection may vary from chronic or subacute infections to sepsis. Prolonged treatment with penicillin is typically recommended for all forms of Actinomyces infections. Parenteral penicillin therapy for 4 weeks–6 weeks, followed by oral use for a couple of months, is recommended [6,17]. Doxycycline is an alternative for whom penicillin is unavailable [6]. Progression of the existing infection and worsening in clinical findings have been described in case reports when empirically initiating treatment with other broad-spectrum antibiotics [8]. Indeed, rapid improvement was observed when anti-biotherapy was switched to penicillin. Drainage is recommended in the presence of an abscess. Antibiotherapy should not be neglected again after drainage. Giving only medical treatment may be considered in cases where drainage is inappropriate.
Conclusion
We reported a rare observation of HA-mimicking cancer. Clinical and radiological observations do not always provide specific information to make an accurate diagnosis. Therefore, a definitive diagnosis can only be made by examining tissue samples. As long as his medical history and physical examination were unremarkable for predisposing features (history of diabetes mellitus, hypertension, alcohol consumption or smoking, etc.), abdominal surgery or immunodeficiency, occupational exposure as a cattle breeder may be the only risk factor for him although we do not know the mechanism. Through our case, we aim to highlight the importance of the suspicion of HA, given the harm of unnecessary surgical approaches and even empirical treatments.
Acknowledgments
Informed consent was obtained orally from the patient before documentation of this case report. Ultrasound images are not available in the computerized system of the hospital. We apologise that we could not reach the Gram-stained samples but the pathologic images are equivalently diagnostic.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch Intern Med. 1975;135(12):1562–1568.
- Alamillos-Granados FJ, Dean-Ferrer A, García-López A, López-Rubio F. Actinomycotic ulcer of the oral mucosa: an unusual presentation of oral actinomycosis. Br J Oral Maxillofac Surg. 2000;38(2):121–123.
- Yamada H, Kondo S, Kamiya J, Nagino M, Miyachi M, Kanai M, et al. Computed tomographic demonstration of a fish bone in abdominal actinomycosis: report of a case. Surg Today. 2006;36(2):187–189.
- Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender. Case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008;12(4):358–362.
- Somsouk M, Shergill AK, Grenert JP, Harris H, Cello JP, Shah JN. Actinomycosis mimicking a pancreatic head neoplasm diagnosed by EUS-guided FNA. Gastrointest Endosc. 2008;68(1):186–187.
- Chegini Z, Didehdar M, Tabaeian SP, Khoshbayan A, Shariati A. A systematic review of case reports of hepatic actinomycosis. Orphanet J Rare Dis. 2021;16(1):192.
- Sharma S, Hashmi MF, DJ Valentino III. Actinomycosis [Internet]. Retrieved 2020. Treasure Island (FL): Stat Pearls Stat Pearls Publishing; 2020.
- Wong JJ, Kinney TB, Miller FJ, Rivera-Sanfeliz G. Hepatic actinomycotic abscesses: diagnosis and management. AJR Am J Roentgenol. 2006;186(1):174–176.
- Ávila F, Santos V, Massinha P, Pereira JR, Quintanilha R, Figueiredo A, et al. Hepatic Actinomycosis. GE Port J Gastroenterol. 2015;22(1):19–23.
- Pulverer G, Schütt-Gerowitt H, Schaal KP. Human cervicofacial actinomycoses: microbiological data for 1997 cases. Clin Infect Dis. 2003;37(4):490–497.
- Castro LL, Cabral MMDÁ, Andrade RFM, Buzatti KCDLR, Silva RGD. Actinomycosis mimicking colonic neoplasia. J. Coloproctol. (Rio J.). 2012;32(3):312–315.
- Hajri M, Omrani S, Ferjaoui W, Mestiri H, Bayar R. Actinomycosis mimicking a pancreatic head neoplasm: A case report. Int J Surg Case Rep. 2022;91:106794.
- Graybill JR, Silverman BD. Sulfur granules: Second Thoughts. Arch Intern Med. 1969;123(4):430–432.
- Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183-197.
- Ab Ahad W, Kumar S, Lone HA, Beghum R. Clinical management of bovine actinomycosis (Lumpy Jaw) in cattle: A case report. IJESC. 2020;10(3):24868–24870.
- Metgud SC, Sumati H, Sheetal P. Cutaneous actinomycosis: A rare case. Indian J Med Microbiol. 2007;25(4):413–415.
- Maraki S, Mavromanolaki VE, Stafylaki D, Anagnostopoulou E, Moraitis P, Kasimati A, et al. A 60-Year Literature Review on Hepatic Actinomycosis. Med Princ Pract. 2022;31(2):103–110.
Keywords
Malignancy, Actinomycosis, Liver abscess, Infection, Liver imaging, Pathology
Cite this article
Akay S, Özamrak BG, Arici Z, Ünal OU. Hepatic Actinomycosis mimics malignancy. Clin Oncol J. 2023;4(1):1–4.
Copyright
© 2023 Seval Akay. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).