Thyroid Gland’s Metastasis of Uterine Leiomyosarcoma
* William Sergi;
Stefano Garritano;
Ivan Botrugno;
Ambra Chiappini;
Carlo Olla Atzeni;
Eupremio Greco;
Giovanni Serio;
Marcello Spampinato;
-
* William Sergi: Department of General Surgery, “Vito Fazzi” Hospital, Lecce, Italy.
-
Stefano Garritano: Department of General Surgery, “Vito Fazzi” Hospital, Lecce, Italy.
-
Ivan Botrugno: Department of General Surgery, “Vito Fazzi” Hospital, Lecce, Italy.
-
Ambra Chiappini: Department of General Surgery, “Vito Fazzi” Hospital, Lecce, Italy.
-
Carlo Olla Atzeni: Department of Pathology, “Vito Fazzi” Hospital, Lecce, Italy.
-
Eupremio Greco: Division of Endocrinology, “Vito Fazzi” Hospital, Lecce, Italy.
-
Giovanni Serio: Department of Pathology, “Vito Fazzi” Hospital, Lecce, Italy.
-
Marcello Spampinato: Department of General Surgery, “Vito Fazzi” Hospital, Lecce, Italy.
-
Nov 15, 2022 |
-
Volume: 3 |
-
Issue: 2 |
-
Views: 2123 |
-
Downloads: 2147 |
Abstract
Introduction: Cancer metastasis to the thyroid gland from other sites is rare.
Case Presentation: a 59-year-old female with a previous history of uterine leiomyosarcoma presented with a plongeant toxic multinodular goiter.
Clinical Discussion: a total thyroidectomy was performed. The diagnosis of metastatic uterine leiomyosarcoma was made, in view of the patient’s history, based on morphological and immunohistochemical findings.
Conclusion: a multidisciplinary approach needs to consider metastatic neoplasms of the thyroid, especially when a previous history of tumor exists or is suspected.
The paper has been written in line with the SCARE criteria. Consent to data processing for scientific purposes is requested and signed at the time of admission and kept in the medical record; the authors confirm that the patient’s parents have signed consent to the publication of the data.
Abbreviations
CT: Computed Tomography; LMS: Leiomyosarcoma; MTC: Medullary Thyroid Carcinoma; SMA: Smooth Muscle Actin; TAHBSO: Total Abdominal Hysterectomy and Bilateral Salphingo-Opherectomy; UTC: Undifferentiated Thyroid Carcinoma
Introduction
Approximately 2%–3% of all thyroid neoplasms are secondary to metastasis: most frequently, there are adenocarcinomas from the kidney, breast, or lungs, and squamous cells carcinomas, mostly from the head and neck; rarely from leiomyomas and leiomyosarcomas [1–3]. Uterine leiomyosarcoma (LMS) is a rare, aggressive tumor with the propensity for distant metastasis [4, 5]: its metastasis to the thyroid gland account only for 1% of the reported cases [6]. It can present as single or multiple lesions, and it is well documented that thyroid metastases may mimic primary thyroid malignancies. As per our knowledge, there have been less than ten reported cases of this malignancy with metastasis to the thyroid gland [2,7]. Correlation with clinical history and radiological findings are crucial to establishing the diagnosis of metastatic leiomyosarcoma. The treatment depends on whether the metastasizing tumor is widespread or isolated, but prognosis and survival rates are poor [7]. We present this case of a metastatic uterine leiomyosarcoma to the thyroid to review the differential diagnosis of spindle cell neoplasms.
Case Presentation
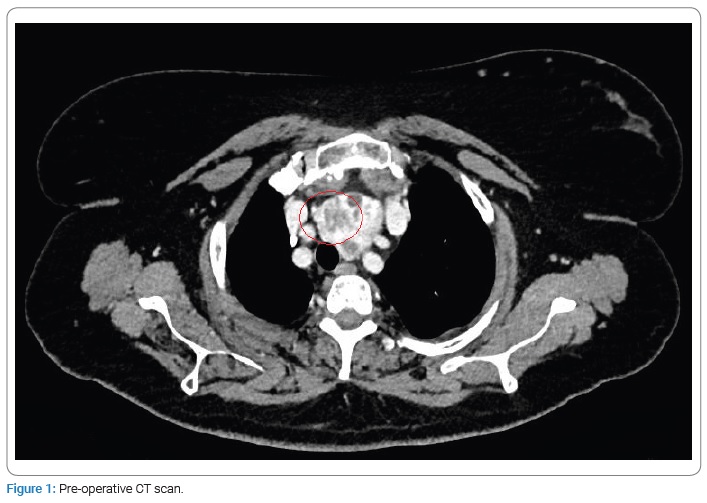
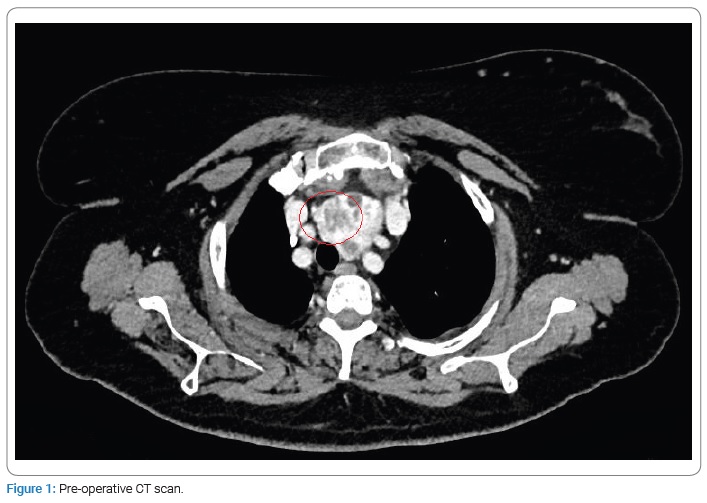
An Endocrinologist followed a 59-year-old woman for a plongeant toxic multinodular goiter with rapidly increasing size. The patient had a previous history of uterine leiomyosarcoma with no metastases, so she underwent a total abdominal hysterectomy and bilateral Salpingo-oophorectomy two years ago in another center. On a CT scan of the neck, the trachea was displaced, but no cervical lymphadenopathy was noted (Figure 1).
After a multidisciplinary discussion, she was admitted to our Department, and a total thyroidectomy was subsequently performed. Postoperatively, the patient as well, and she was discharged on day 2 with a suppression dose (50 mcg) of thyroxine suggested by the Endocrinologist.
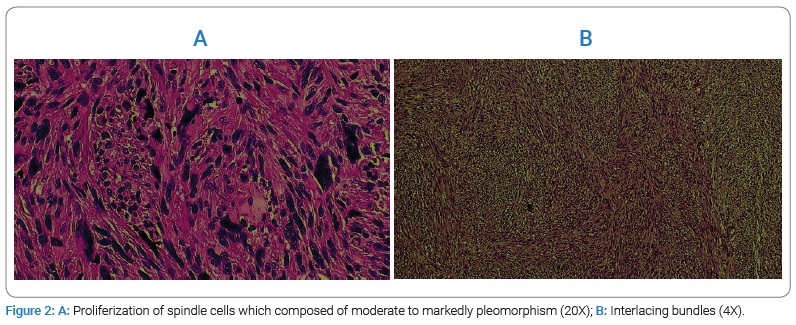
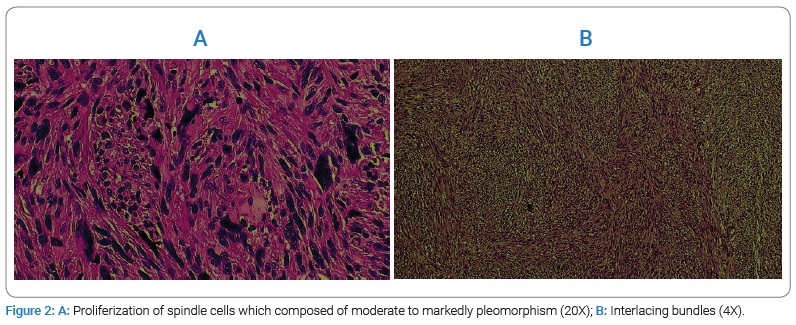
Pathology: At the macroscopical examination, the thyroid shows a multilobular pattern with the right lobe’s greatest node (4 cm maximum diameter). At the microscopic examination, this node is characterized by a proliferation of spindle cells which are composed of moderate to markedly pleomorphism, arranged in interlacing bundles with eosinophilic cytoplasm and hyperchromatic nuclei (Figure 2A,B).
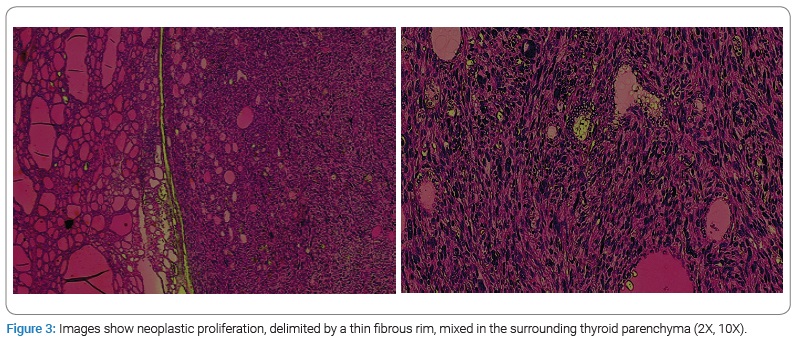
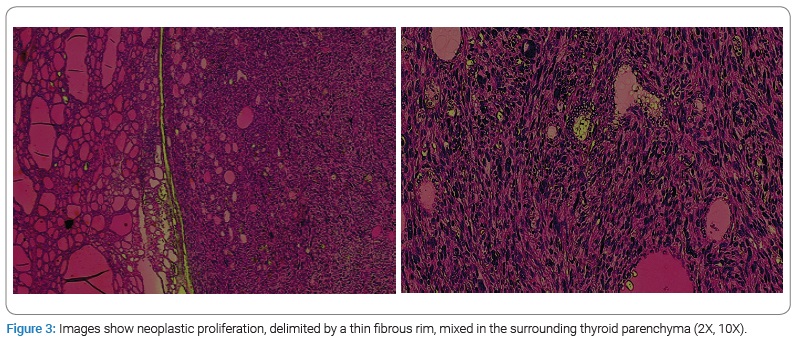
The neoplastic proliferation, albeit delimited by a thin fibrous rim, was mixed in the surrounding thyroid parenchyma in several areas (Figure 3).
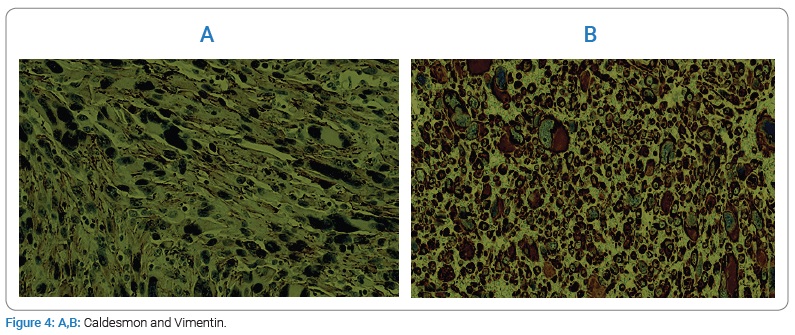
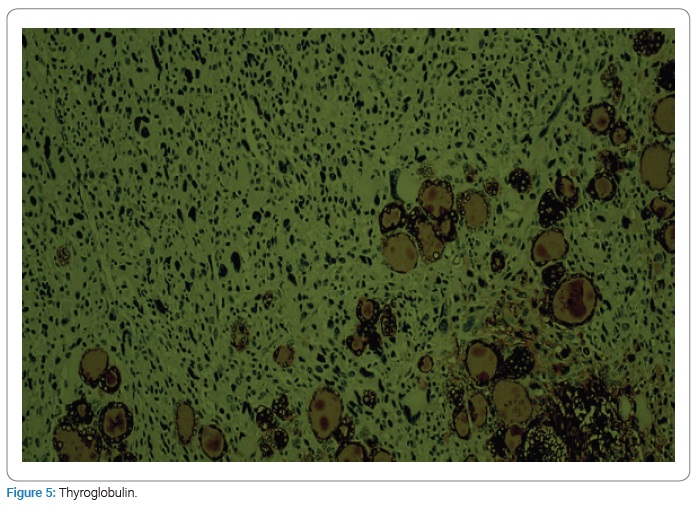
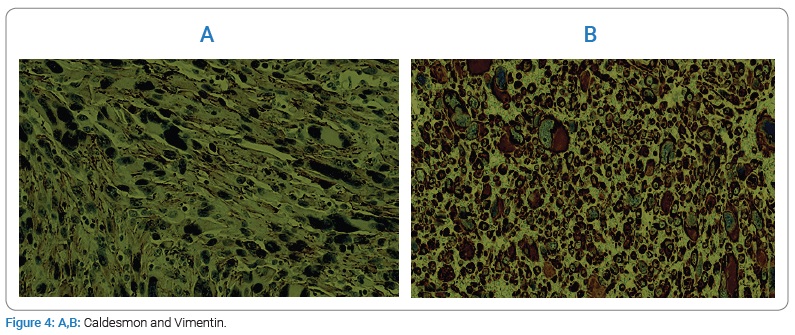
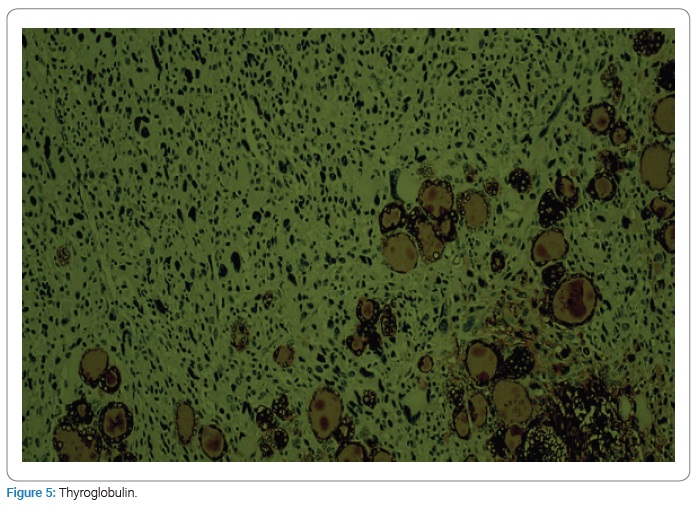
The neoplastic cells are positive for caldesmon and vimentin (Figure 4A,B); occasional positivity of smooth muscle actin (SMA), and negative for desmin, thyroglobulin (Figure 5), CKAE1/AE3, HMB45, S100, chromogranin and calcitonin.
Morphological and immunohistochemical findings confirm the diagnosis of high-grade leiomyosarcoma.
In this situation, it becomes impossible to determine whether the thyroid tumor is a metastasis or a second primary. However, the previous history of uterine leiomyosarcoma suggests a thyroid localization of this tumor.
Discussion
Tumors metastasizing to the thyroid are less than 0.1% of all thyroid neoplasms. Metastatic uterine leiomyosarcoma of the thyroid is a very rare entity. Its clinical presentation is similar to primary thyroid tumors: patients usually show a thyroid mass accompanied by compressive symptoms; hoarseness of voice, dysphagia, dyspnoea, and weight loss can be associated [8]. However, the sudden appearance of a thyroid mass after the diagnosis of a primary tumor most likely indicates the secondary involvement of the thyroid [9].
Radiologically, there are no specific sonographic findings for a metastatic thyroid nodule. However, unilateral or bilateral multiple suspected thyroid nodules without evidence of microcalcification on ultrasonography may be suggestive of metastatic nodules among patients with a known primary tumor [10].
The differential diagnoses of spindle cell tumors of the thyroid include undifferentiated (anaplastic) thyroid carcinoma (UTC) with a sarcomatoid pattern, medullary thyroid carcinoma (MTC) with spindle cells morphology, and spindle cell tumor with thymus-like differentiation (SETTLE); positive expression of myogenic markers and negative expression of epithelial markers are very useful in establishing the diagnosis [7].
Preoperative diagnosis of leiomyosarcoma of the thyroid needs a team of surgeons, radiologists, and pathologists: correlation with clinical-radiological findings and a multidisciplinary approach are needed in complimentary to histopathological diagnosis.
Therapy depends on patient performance status: in the majority of cases, palliative care is the choice of treatment; total thyroidectomy or lobectomy (without neck dissection) is aimed at local disease control and long-term cure in selected patients [8,9].
Conclusion
In conclusion, we described a rare case of metastatic uterine leiomyosarcoma to the thyroid gland with a coexisting multinodular goiter in a patient with no other metastases at the time of thyroidectomy. Unfortunately, diagnosing metastasis to the thyroid gland can be difficult, and it is associated with a poor prognosis.
A detailed history, physical examination, and knowledge of the differential diagnoses and their presentations can be very useful in order to differentiate primary thyroid neoplasms such as metastatic tumors pertaining to the treatment of aggressive distant metastatic disease.
Acknowledgments
Author contribution: William Sergi: Design of work and manuscript writing; Stefano Garritano: Co-author; Ivan Botrugno, Giovanni Serio, Ambra Chiappini: Review of literature; Carlo Olla Atzeni, Eupremio Greco: Authors of discussion; Marcello Spampinato: supervisor; Guarantor: Spampinato Marcello; Registration of research studies: The submitted case report is not a research study; Provenance and peer review: Not commissioned, externally peer-reviewed.
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Ethical approval: In our institute, the approval of the ethics committee for the retrospective analysis of a clinical case report is not required.
Sources of funding: No fundings were used.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group. The SCARE 2020 guideline: updating consensus surgical CAse Report (SCARE) guidelines. Int J Surg. 2020; 84:226–230.
- Eloy JA, Mortensen M, Gupta S, Lewis MS, Brett EM, Genden EM. Metastasis of uterine leiomyosarcoma to the thyroid gland: case report and review of the literature. Thyroid. 2007;17(12):1295–1297.
- Zhang L, Liu Y, Li X, Gao W, Zheng C. Metastases to the thyroid gland: A report of 32 cases in PUMCH. Medicine (Baltimore). 2017;96(36):e7927.
- Vellanki VS, Rao M, Sunkavalli CB, Chinamotu RN, Kaja S. A rare case of uterine leiomyosarcoma: a case report. J Med Case Rep. 2010;4:222.
- Leath CA 3rd, Huh WK, Straughn JM Jr, Conner MG. Uterine leiomyosarcoma metastatic to the thyroid. Obstet Gynecol. 2002;100(5 Pt 2):1122–1124.
- Tirumani SH, Deaver P, Shinagare AB, Tirumani H, Hornick JL, George S, et al. Metastatic pattern of uterine leiomyosarcoma: retrospective analysis of the predictors and outcome in 113 patients. J Gynecol Oncol. 2014;25(4):306–312.
- Nemenqani D, Yaqoob N, Khoja H. Leiomyosarcoma metastatic to the thyroid diagnosed by fine needle aspiration cytology. J Pak Med Assoc. 2010;60(4):307–309.
- Nixon IJ, Coca-Pelaz A, Kaleva AI, Triantafyllou A, Angelos P, Owen RP, et al. Metastasis to the thyroid gland: a critical review. Ann Surg Oncol. 2017;24(6):1533–1539.
- Nakhjavani MK, Gharib H, Goellner JR, van Heerden JA. Metastasis to the thyroid gland. A report of 43 cases. Cancer. 1997;79(3):574–578.
- Chung SY, Kim EK, Kim JH, Oh KK, Kim DJ, Lee YH, et al. Sonographic findings of metastatic disease to the thyroid. Yonsei Med J. 2001;42(4):411–417.
Keywords
Leiomyosarcoma; Metastatic thyroid cancer; Multinodular goitre
Cite this article
Sergi W, Garritano S, Botrugno I, Chiappini A, Atzeni CO, Greco E, et al. Thyroid gland’s metastasis of uterine leiomyosarcoma. Clin Oncol J. 2022;3(2):1–4.
Copyright
© 2022 William Sergi. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).